Case Study: When Hindlimb Lameness Isn’t What It Seems
Physical exam of the hind limb can help localize pain, but imaging is often needed for confirmation.
In referral practice, the most instructive cases aren’t always the most complex. Sometimes they’re the ones that seem clear-cut…until the clinical picture starts to shift. When imaging doesn’t align with neurologic findings, it forces us to pause, reassess, and look beyond what we expect to see.
This case explores that pivot point. The turning moment when a normal scan doesn’t explain the pain. When the reflex to move forward is replaced by a better question: Are we looking in the right place—and with the right tool?
At SAGE Teleradiology, we regularly evaluate patients whose clinical signs blur the line between orthopedic and neurologic disease. And often, the most valuable images are the ones that reshape and give a new diagnosis.
[Contact our team] to submit a case and consult with our board-certified specialists!
In This Article:
Boxers are energetic, muscular dogs often seen in neurology and orthopedic referral cases.
Case Overview
Patient: Delta Belle, 5-year-old spayed female Boxer
Primary Complaint: Acute left hind limb lameness
Symptoms: Crying out, unable to rest comfortably, guarding posture
Pain Response: Significant discomfort with lumbosacral (LS) pressure and hip extension
Initial Concern: Suspected orthopedic or spinal pathology
Delta Belle arrived for evaluation after a sudden onset of severe left hind limb lameness. She was painful, reactive to movement, and unable to find a comfortable position.
Based on the acuity and severity of pain, an orthopedic condition (e.g. hip dysplasia, stifle injury, or iliopsoas strain) was considered. However, radiographs and an orthopedic exam ruled out joint disease.
Transverse and sagittal CT images of the lumbosacral spine in a dog, showing no evidence of compression.
Referral to a neurologist for a CT scan revealed a more puzzling finding: a severely decreased left patellar reflex with normal withdrawal, suggesting femoral nerve or L4–L6 spinal cord involvement. Pain on LS pressure further raised suspicion for spinal nerve root compression.
Clinical Workup & Localization
While orthopedic disease was excluded, pain remained localized to the lumbosacral (LS) region. This case began with reasonable orthopedic suspicion. The nature of the lameness, patient discomfort, and pain on hip extension mimicked stifle or hip disease. When those possibilities were excluded, focus shifted to potential lumbosacral or femoral nerve pathology.
The reflex asymmetry pointed to a lower motor neuron lesion, and the normal withdrawal reflex helped narrow localization to the femoral nerve or its spinal cord origin. Given the lack of compressive lesions on CT, MRI was recommended to evaluate the spinal cord, nerve roots, and surrounding soft tissues in greater detail.
✎ Radiologist’s Note:
When pain localizes to the LS region but spinal imaging is inconclusive, consider extraneural soft tissue structures—especially in large-breed, athletic dogs where iliopsoas injuries are increasingly recognized.
Imaging Findings
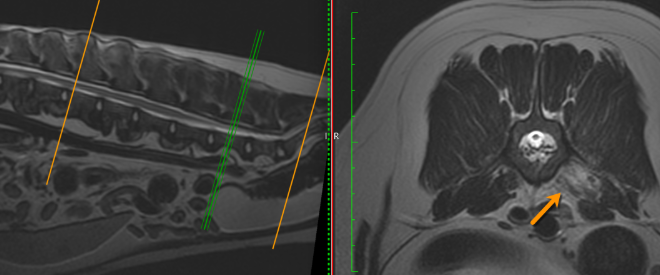
STIR MRI reveals focal hyperintensity in the left iliopsoas muscle consistent with acute strain injury.
Delta Belle underwent MRI of the lumbar spine using STIR and T2-weighted sequences. Findings included:
Hyperintensity within the left iliopsoas muscle at the level of L5, consistent with acute inflammation and tearing
No compressive lesions in the spinal cord or nerve roots
Normal disc spaces and vertebral alignment
T2-weighted sagittal and axial images show asymmetry and signal change at the left iliopsoas insertion.
These findings confirmed the diagnosis: an acute iliopsoas muscle tear, likely traumatic or strain-related.
✎ Radiologist’s Note
This case is a powerful reminder that spinal pain doesn’t always originate in the spine. Iliopsoas injuries can present with localized pain, abnormal gait, and even reflex changes due to proximity to the femoral nerve.
Clinical Outcome & Treatment Plan
With a definitive diagnosis in hand, Delta Belle’s treatment plan focused on:
Controlled rest and activity restriction
Anti-inflammatory medication
Gradual reintroduction of low-impact exercise and physical therapy
Avoiding unnecessary spinal surgery or invasive diagnostics, the team was able to provide a precise, conservative treatment plan tailored to her injury.
Takeaways for Neurology & Imaging Teams
Not all lameness is orthopedic and not all pain is spinal. When the two overlap, soft tissue injury should remain in the differential.
Iliopsoas injury can mimic LS disease with pain, lameness, and even decreased patellar reflexes.
MRI remains the gold standard for identifying muscle strain, especially when CT and radiographs are inconclusive.
STIR sequences are invaluable for detecting soft tissue inflammation, edema, or tear.
Be prepared for an imaging result that shifts the clinical narrative.
Need Imaging Support on a Challenging Lameness Case?
At SAGE Teleradiology, we support diagnostic clarity for cases where pain and neurologic signs don’t add up. Our high-field MRI interpretations help distinguish spinal cord, nerve root, and soft tissue pathology so your treatment plan starts from a place of certainty.
[Contact our team] to submit a case and consult with our board-certified specialists!