In-House vs. Teleradiology: How to Know When It’s Time to Send the Study Out
When weighing in-house reads against teleradiology, clarity begins with asking the right questions."
The choice between in-house vs. teleradiology isn’t always black and white. In reality, it’s one of the more nuanced decisions clinicians make—especially when imaging findings are subtle, when treatment hinges on the report, or when you’ve seen this case pattern before but still feel that edge of doubt.
This guide breaks down how to think through that decision. Not just in terms of image quality or workflow, but in terms of clinical clarity, team bandwidth, and patient care. Whether you’re in a solo practice managing mixed cases or leading a referral team juggling advanced modalities, your imaging strategy matters.
At SAGE Teleradiology, we don’t just read scans, we help teams read between the lines. Because sometimes the question isn’t what the image shows. It’s what it means for your patient.
This Blog Covers:
Key questions to ask before sending veterinary imaging to teleradiology
When in-house interpretation makes sense—and when it doesn’t
How to create a smart, blended diagnostic workflow that supports your team
If you’ve ever hesitated over an equivocal MRI, this guide is for you!
How to Decide Between In-House and Teleradiology Interpretation
Not every study needs to be sent out, and knowing when to read confidently in-house is a critical skill. In fact, for many clinics, in-house interpretation is the backbone of efficient case management. It saves time, preserves budget, and reinforces the diagnostic confidence of your team.
In-house reads are especially appropriate when:
The findings are classic, overt, and line up neatly with the clinical picture.
The anatomic region is one you encounter routinely: thoracolumbar spine, stifles, elbows.
You’ve seen the same pattern dozens of times, and the interpretation doesn’t hinge on subtlety.
The case is time-sensitive (e.g., ER setting), but not high-stakes in complexity.
A Common Example:
A middle-aged Dachshund presents acutely paraplegic. MRI shows a large, classic extradural compression at T12–13. No signal change, no ambiguity, no unexpected findings. You’ve treated this scenario before. The imaging confirms what you already suspect from the neuro exam. In this case, sending to teleradiology won’t necessarily change your decision or outcome, and that’s perfectly appropriate.
The key is knowing when the image tells a complete story—and when it’s only the first chapter.
When Should You Send Veterinary Imaging to Teleradiology?
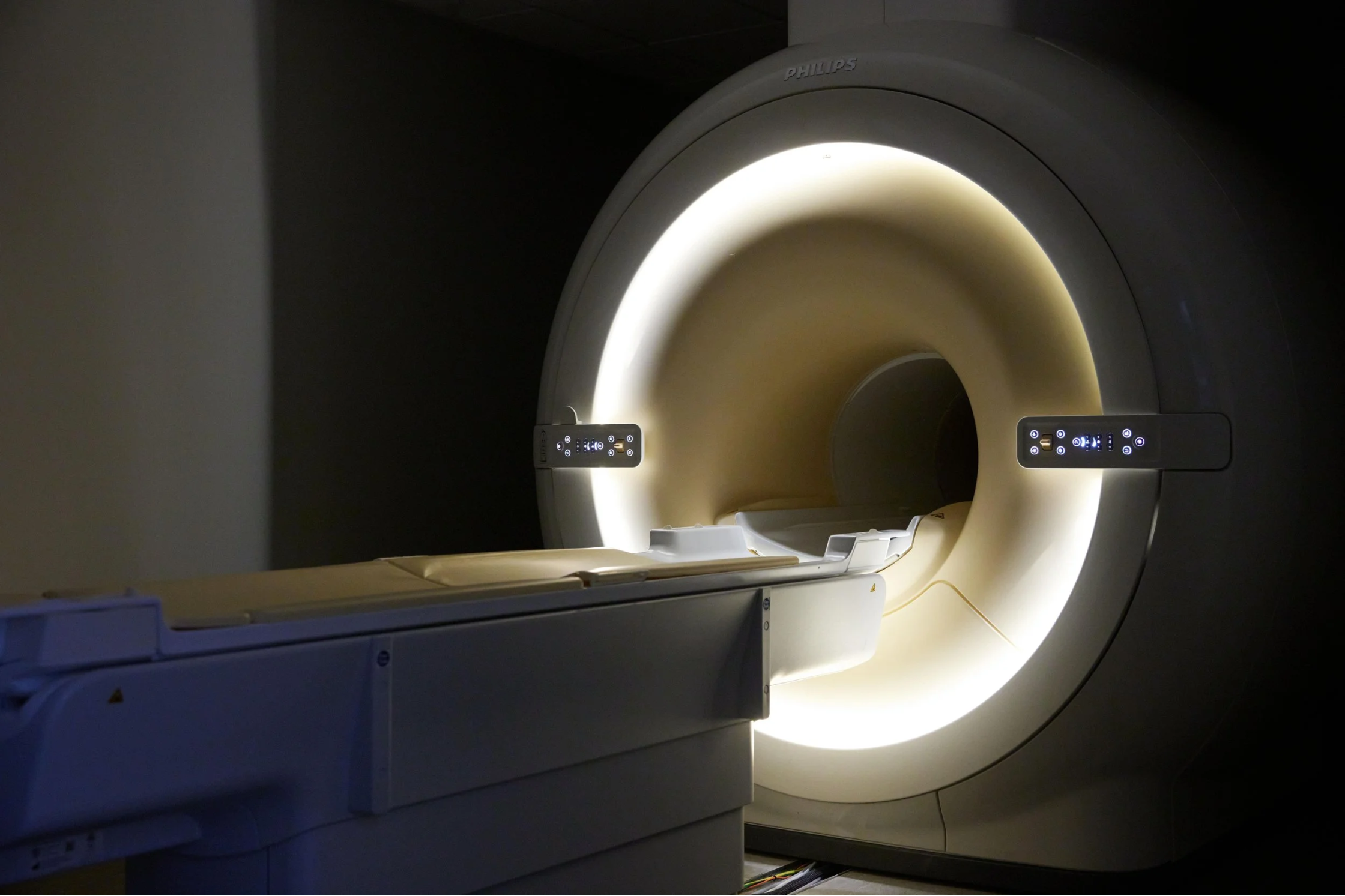
Our high-field MRI machine: a tool for advanced imaging and expert teleradiology review.
Teleradiology isn’t a replacement for your expertise. Think of it as an extension of it. Especially with advanced modalities like high-field MRI or CT, some findings are nuanced, easily missed, or require context that only comes with deep subspecialty focus. In these moments, a second set of highly trained eyes doesn’t slow you down—it sharpens your direction.
Teleradiology is most valuable when:
The findings are subtle, bilateral, or ambiguous
You’re navigating a modality with steep interpretive demands (e.g., neuro MRI, triple-phase CT)
The case involves complex or region-specific anatomy (nerve roots, stifles, inner ear, brachial plexus)
You’re deciding between surgical and medical management, and imaging is the pivot point
You need to strengthen communication with clients or the referring team—or reduce medicolegal risk
In these cases, subspecialty input gives you accuracy and confidence in what comes next.
A Practical Decision Checklist: Should I Send This Case Out?
Before deciding on whether to send your case out, know where to start asking questions.
Not every case needs a second opinion—but some clearly benefit from one. Use this FAQ-style guide to help decide when a case might warrant teleradiology referral:
Is the study clearly diagnostic in my hands?
If not—send it. Ambiguity is a risk you don’t need to carry alone.
Are the findings subtle, symmetric, or just not adding up?
When you’re unsure, escalation protects both your patient and your plan.
Is this a high-field MRI or contrast-enhanced CT?
These modalities often benefit from pattern recognition that comes with volume and specialization.
Will this interpretation directly impact surgery, referral, or treatment decisions?
A second opinion adds clarity and clinical alignment when outcomes are on the line.
Has the case been read as normal, but signs persist—or treatment failed?
A fresh review may pick up what was missed the first time.
Would subspecialty input support your client communication or referral conversations?
Our reports are designed to back your clinical plan—not just describe anatomy.
Do you have the time and bandwidth to dig deep into this case today?
If not, let us handle the review while you stay focused on care.
How fast do you need an answer?
We offer same-day and 24-hour turnaround, so you don’t have to choose between speed and depth.
Is veterinary MRI interpretation better with a specialist?
When the modality is complex, the findings subtle, or the anatomy advanced—yes. Subspecialty input often changes outcomes.
What’s the difference between general teleradiology and subspecialist interpretation?
General services may provide findings. Subspecialists connect those findings to treatment logic, patient context, and your next steps.
Still unsure?
If you’re asking whether it’s worth sending—that’s often the sign you should.
Case Example: When “Unremarkable” Isn’t Enough
A second review revealed subtle signal change at the L6 nerve root, guiding successful surgery.
A 6-year-old Labrador presented with subtle left hind limb lameness. The initial high-field MRI was interpreted as unremarkable, but the surgeon remained uncertain and requested a second opinion.
On re-review, we identified a faint, localized signal change at the left L6 nerve root. It was subtle but matched the neurologic findings. The surgeon proceeded with a focused decompression, and the patient made a full recovery.
Without subspecialty input, this case would likely have been managed medically, with ongoing discomfort and delayed resolution. In this scenario, expert review didn’t just confirm the diagnosis—it changed the course of care.
Blending Both Approaches: The Smart Workflow
The smartest clinics don’t rely 100% on either in-house or teleradiology. They triage strategically:
Some studies stay in-house, but complex or high-impact cases benefit from a review with SAGE Teleradiology.
This approach saves time, supports better decisions, and creates consistency in care.
Conclusion: It’s Not a Question of If You Can Read It—But Should You
You’re a skilled clinician. You can interpret imaging. But advanced imaging isn’t just about being capable—it’s about being certain.
We’re here to support your clinical instincts, not override them. We recognize subtle patterns, interpret rare presentations, and align our reads with your diagnostic and therapeutic goals. Not every case needs a subspecialist read. But when it does, it can change everything!
Ready for backup on your next tough case?
[Send us a case.] We’ll help you see it clearly within 24 hours.